HOW IS POP TREATED?
While POP is not life threatening and your symptoms may be minimal, there are treatment options available.
Lifestyle changes
You can avoid excessive straining from chronic constipation and heavy lifting, and lose weight to avoid additional physical stress on the pelvic organs.
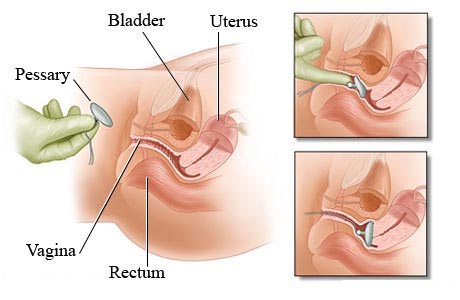
Vaginal pessary
A pessary is a silicone device inserted into the vagina to support the bladder and urethra as well as relieve pressure on the bladder and rectum. Pessaries help prevent the prolapse from moving down. We can teach you how to properly insert and remove the pessary if you choose to use one.
Pelvic floor physical therapy
Strengthening the muscles that help elevate and lift the pelvic organs can help prevent worsening of POP. Working with a physical therapist who specializes in pelvic health can improve your strength to support the viscera (internal organs within the pelvis). Physical therapy will also incorporate safe exercises to help alleviate any symptoms.
Prolapse surgery
There are several ways surgery can help repair POP:
Apical suspensions, to support the top of the vagina, can be done at the same time as a hysterectomy. There are two types of this surgery:
- sacral colpopexy, performed robotically or laparoscopically through an abdominal incision to attach mesh material from the vagina to a ligament near the tailbone; or
- uterosacral or sacrospinous ligament suspension, the suturing of the top of the vagina to a ligament in the pelvis done through the vagina.
Anterior vaginal prolapse repair uses sutures, mesh or a graft to correct a cystocele/bladder prolapse through an incision in the wall between the vagina and the bladder.
Posterior vaginal prolapse repair uses sutures, mesh or a graft to correct a rectocele/rectal prolapse through an incision between the wall of the vagina and rectum.
TERMS:
Cystocele: the bladder descending or falling into the anterior (front) wall of the vagina, creating a bulge.
Enterocele: the small bowel pushing into the vagina, usually due to a weakening of the upper vaginal wall.
Rectal prolapse: when the rectum falls out of the anus.
Rectocele: the rectum descending into the posterior (back) wall of the vagina, creating a bulge.
Uterine prolapse: when the uterus falls out of the vagina because of weakness in the ligaments that support the top of the vagina.
|
KEY POINTS
1. POP is the descending of the bladder, uterus and/or rectum due to loss of ligament and muscle support.
2. Symptoms are sometimes minimal or absent and are not life-threatening
3. Treatment options include conservative management or surgery.
|
Download the Educational PDF